Insulin Resistance: The Silent Driver Behind Cholesterol Problems
Share
When people think about heart health, cholesterol usually takes center stage.
Doctors talk about LDL, HDL, and triglycerides. Friends might mention “good” versus “bad” cholesterol. But if you pull back the curtain, there’s something deeper at play that explains why cholesterol numbers go haywire in the first place: insulin resistance.
This isn’t just a medical buzzword. Insulin resistance is one of the most important—and most overlooked—factors in modern health. It shapes how your body handles sugar, fat, and energy. It ties directly into obesity, type 2 diabetes, and cardiovascular disease. Understanding it could make the difference between staying healthy into old age or struggling with decades of preventable problems.
What Is Insulin, and Why Does It Matter?
Insulin is a hormone produced by the pancreas. Its main job is simple: when you eat carbs, they break down into glucose (sugar) in your blood. Insulin’s job is to unlock your cells so glucose can move inside and be used for energy. Think of insulin as the key, and your cells as the lock.
Without insulin, glucose stays stuck in the bloodstream, which is toxic over time. With insulin, glucose gets cleared, your energy levels stay stable, and your metabolism runs smoothly.
How Resistance Develops
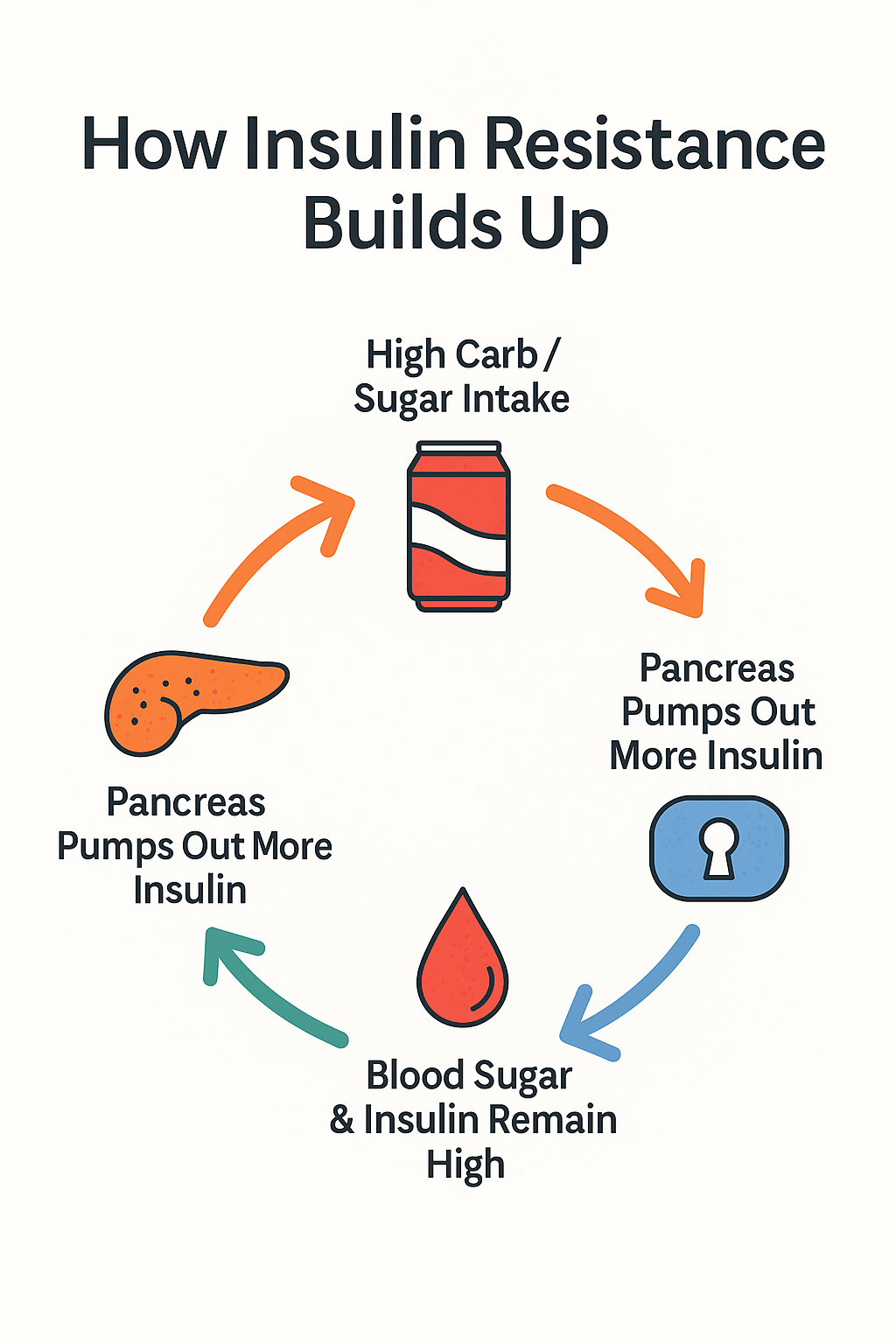
The problem comes when insulin shows up too often. A diet high in refined carbs—bread, pasta, soda, desserts—forces your pancreas to pump out insulin day after day. Over time, your cells get “tired” of listening. They stop responding to insulin’s signal.
Now you have two issues:
-
Glucose remains high in your blood → raising your blood sugar.
-
Insulin stays elevated → a state called hyperinsulinemia.
It’s a vicious cycle. The more resistant your cells become, the harder your pancreas works to flood your system with even more insulin. Eventually, this overdrive burns out your system and blood sugar rises out of control.
What Insulin Resistance Does to Cholesterol
Here’s where cholesterol enters the story. High insulin levels trigger a cascade of changes in your blood chemistry:
-
Triglycerides increase. The liver turns excess sugar into fat, releasing triglycerides into the bloodstream.
-
HDL (“protective” cholesterol) drops. This removes the cleanup crew that normally clears cholesterol from arteries.
-
LDL particles become small and dense. These tiny particles are more likely to slip into artery walls and form plaque.
In short: insulin resistance is the hidden force that transforms cholesterol from useful to dangerous. A cholesterol test alone might not reveal the whole story, but if triglycerides are up and HDL is down, insulin resistance is usually behind it.
Beyond Cholesterol: The Wider Damage
Insulin resistance doesn’t stop at cholesterol. It drives a cluster of problems known as metabolic syndrome, including:
-
Abdominal fat (the “spare tire”)
-
High blood pressure
-
High fasting glucose
-
Chronic inflammation
Together, these changes accelerate the risk of heart disease, stroke, fatty liver disease, and type 2 diabetes. Even before diagnosis, people often notice fatigue, brain fog, sugar cravings, and difficulty losing weight.
Who Should Worry?
Insulin resistance often starts silently, years before blood sugar looks abnormal on a lab test. Warning signs include:
-
Waist circumference over 40 inches for men or 35 inches for women
-
Triglycerides above 150 mg/dL
-
HDL below 40 mg/dL in men or 50 mg/dL in women
-
Fasting glucose creeping above 100 mg/dL
-
High blood pressure
You don’t need all of these to be at risk. Even one or two can suggest early insulin resistance.
Can It Be Reversed?
The encouraging news: insulin resistance isn’t permanent. With consistent lifestyle changes, many people dramatically improve their insulin sensitivity within months. Here’s what research shows helps most:
-
Cut refined carbs and sugar. Reduce foods that spike glucose quickly—soda, pastries, candy, white bread, and pasta.
-
Prioritize protein and healthy fats. Eggs, fish, nuts, olive oil, and avocado help stabilize blood sugar and reduce cravings.
-
Increase fiber. Vegetables, beans, and whole foods slow digestion and improve insulin sensitivity.
-
Time your meals. Giving your body longer breaks between meals (intermittent fasting) lowers insulin exposure.
-
Move daily. Muscle activity soaks up glucose without needing insulin. Both resistance training and walking after meals are effective.
-
Sleep and stress management. Poor sleep and chronic stress raise cortisol, which worsens insulin resistance.
-
Lose visceral fat. Even a 5–10% weight reduction can significantly improve insulin response.
Why This Matters to Cholesterol Testing
If you’ve ever been surprised by high cholesterol numbers, especially high triglycerides with low HDL, insulin resistance may be the real issue. Simply lowering cholesterol with medication doesn’t fix the root cause. The real target should be improving insulin sensitivity.
For medical practitioners, this means looking beyond LDL levels and screening for markers of metabolic health. For younger adults, it means realizing that insulin resistance doesn’t just appear “later in life.” It starts with lifestyle choices now.
The Takeaway
Insulin resistance is the quiet engine driving many modern health problems. It distorts cholesterol, fuels inflammation, and sets the stage for heart disease and diabetes. The good news? It’s reversible—if you catch it early and make changes.
The next time you see a cholesterol test result, remember: the numbers might only be the smoke. Insulin resistance is often the fire.
